ROLE OF BODY MASS INDEX IN THE DEVELOPMENT OF POST-DURAL PUNCTURE HEADACHE IN OBSTETRIC ANESTHESIA DURING CESAREAN-SECTIONS
https://doi.org/10.5281/zenodo.17400627
DOI:
https://doi.org/10.64105/s2pt7q36Keywords:
Post-Dural Puncture Headache, Csf Leakage, Spinal Anesthesia, State-Trait Anxiety Inventory, Prior Exposure.Abstract
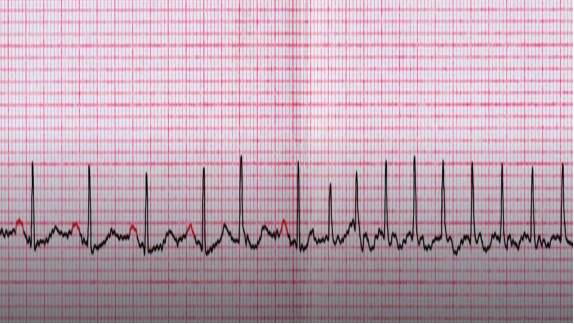
Post-Dural Puncture Headache (PDPH) is a prevalent complication in obstetric anesthesia, particularly following spinal anesthesia for cesarean sections, affecting patient recovery and quality of life due to CSF leakage and orthostatic symptoms. This cross-sectional descriptive study, conducted over four months at Rehman General Hospital, Samar Bagh, Dir, aimed to investigate the prevalence and determinants of PDPH among 370 obstetric patients aged 18-45 years undergoing elective cesarean sections under spinal anesthesia, focusing on factors like BMI, maternal age, needle characteristics, and comorbidities. Using simple convenient sampling, data were collected via a structured questionnaire and the State-Trait Anxiety Inventory (STAI), analyzed with SPSS version 23.0 employing descriptive statistics, paired t-tests, and Chi-square tests for significance (p < 0.05). Results revealed that 72.4% of patients were aged 18-30, 58.8% had normal BMI, 40.4% had prior spinal anesthesia exposure, and 41.7% reported headaches, with 34.8% experiencing posture-related aggravation; blunt-tip, fine-gauge needles (25-27G) were used in 82.1% and 71.4% of cases, respectively, and anesthesia was administered in the sitting position for 98.4%. Discussion highlights that younger age, higher BMI, prior exposure, and procedural factors significantly increase PDPH risk, aligning with studies from Gambia, Ethiopia, and Nigeria, and underscoring gaps in training and guidelines. In conclusion, this research emphasizes the need for precision anesthesia to address modifiable risks, improving maternal outcomes and reducing PDPH burden in obstetric care.